Alliance operations tend to center around a theme. In 2017, we focused
on trust and relationship building by regularly meeting with practitioners
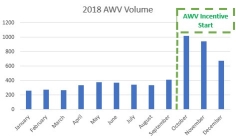
and their office staff. In 2018, our group tested the waters of targeted
incentivization with projects like HCC Risk coding and the Q4 AWV payment
program. This year the Alliance is focused on optimizing workflows so
our network can reach its full potential. This theme has manifested itself
through a series of process redesigns both internally and externally.
Last year’s incentivization programs, while effective (see figure 1),
put significant burden on primary care offices. The programs tended to
require additional documentation and paper work, often in a compressed
time window. This year we have consolidated the incentivized projects
for AWVs, Care Gap Closure, and HCC Risk Coding into one holistic initiative:
The Green Sheet Project. The goal of this project is to incentivize PCPs
to perform key activities on our NextGen ACO patients, while shifting
the lift of documentation and grading to the Alliance’s Clinical
Documentation Specialist (CDS) team.
The project has a relatively simple design: At the start of the year the
Alliance delivers Green Forms to the PCP. Each form represents one NextGen
patient and explains what the Alliance would ideally expect from a provider
during an Annual Wellness Visit (AWV) with that patient. Once a provider
conducts an AWV for a patient, he/she signs and dates the form (no other
documentation is needed). Each quarter the Alliance collects and grades
the completed forms, then pays the office based on their work. The result
is a process where physicians maximize their time performing the value-added
activities, while our team of chart abstractors check for documentation.
Internally, the Alliance has redesigned its care coordination model. Our
analytics team created a pool of high risk NextGen, Anthem, and MWHC Associates
so we can narrow our focus. We then created an efficient workflow by altering
the prior model at three key points.
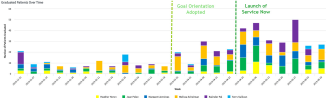
First, we implemented a tool to help our RNCCs self-manage their workflow.
This tool not only automatically assigns patients to the nurses but has
a suite of dashboards to help them manage their patient panel. Next, we
instilled a goal-oriented approach to care management. By focusing on
achieving defined meaningful objectives with the patient, we can confidently
graduate them from our care. Finally, we redesigned our Epic care coordination
module to focus the workflow and reduce documentation. Once again, the
goal is to ensure that our RN care coordinators are working to their full
potential. The impacts of this process improvement project have been significant
(see figure 2).
In 2019, our team is committed to continuing our work to roll out Alliance
projects in a way that ensures providers work at the top of their licenses,
minimizes time crunches, and curbs excess documentation. Ensuring that
we have a network where physicians, nurses, and administration are working
to their full potential is critical to sustaining our success in years to come.