
Alliance Notes on Quality, 2017
Many feel that
Quality as it applies to healthcare is a difficult thing to define. I favor the
following definition from the Institute of Medicine (especially as it
applies to a clinically integrated network like the Alliance dedicated
to promoting Population Health): Quality is
“The degree to which health services for individuals and populations
increase the likelihood of desired health outcomes and are consistent
with current professional knowledge.”
Not only is quality in healthcare difficult to define, it is difficult
to measure and quantify. It reminds me of what Justice Potter Stewart
said about pornography in the famous obscenity case of Jacobellis v.Ohio
in 1964 when he commented that “hard-core pornography” was
hard to define, but that “I know it when I see it”. Things
like compassion, empathy and deductive reasoning are all important features
in caring for patients but are very hard to measure. Our quality measures
need to be discreet, quantifiable, relatively simple to measure and reproducible.
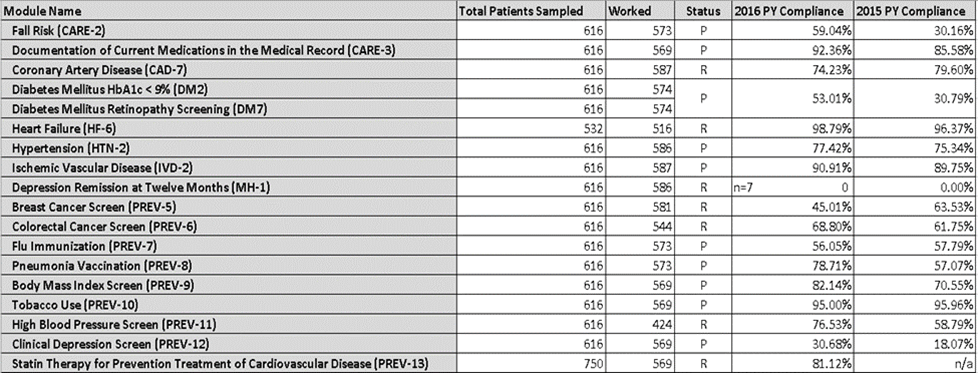
GPRO (Group Practice Reporting Option) measures, which are a component
of the MSSP (Medicare Shared Savings Program) which we have been participating
in since 2015, meet these criteria. The following table documents our
GPRO performance in both 2015 and 2016. The embargo on releasing this
data to the public was recently lifted by CMS and, therefore, you are
now free to discuss this excellent quality performance outside the confines
of the Alliance. The “Status” column shows that 11 of the
18 measures were performance measures in 2016. 2015 was a reporting year
only. “Statin Therapy” was not a reported measure in 2015.
It is apparent that 11 of the measures improved year over year, some dramatically
so (Fall Risk Screening, Composite Diabetes Score and Depression Screening).
The only one that went down significantly was “Breast Cancer Screening”
and this is only because CMS did not accept 3-D mammograms in 2016. 3-D
mammography will be accepted as complying with the measure in 2017.
This improvement is a testament to the Alliance IT team which accurately
quantified our performance, mined real-time data from our EMRs, reported
this to you regularly throughout the year and instructed our practices
on how best to comply with these measures. And, of course, it reflects
our practices and providers having cooperated with our Alliance team in
doing the work necessary and having documented it accurately in their
EMRs. This bodes well for the future success of the Alliance; i.e. that
we can identify opportunities for improvement, put together an appropriate
plan and then put that plan into action. We have made a commitment to
value-based care. As such, our payer partners will continue to monitor
our performance to ensure that we are delivering more efficient care without
compromising the quality of the care we deliver. Our quality performance
to date is testimony to our capacity to do so.