Message from the Medical Director-Richard Lewis, MD
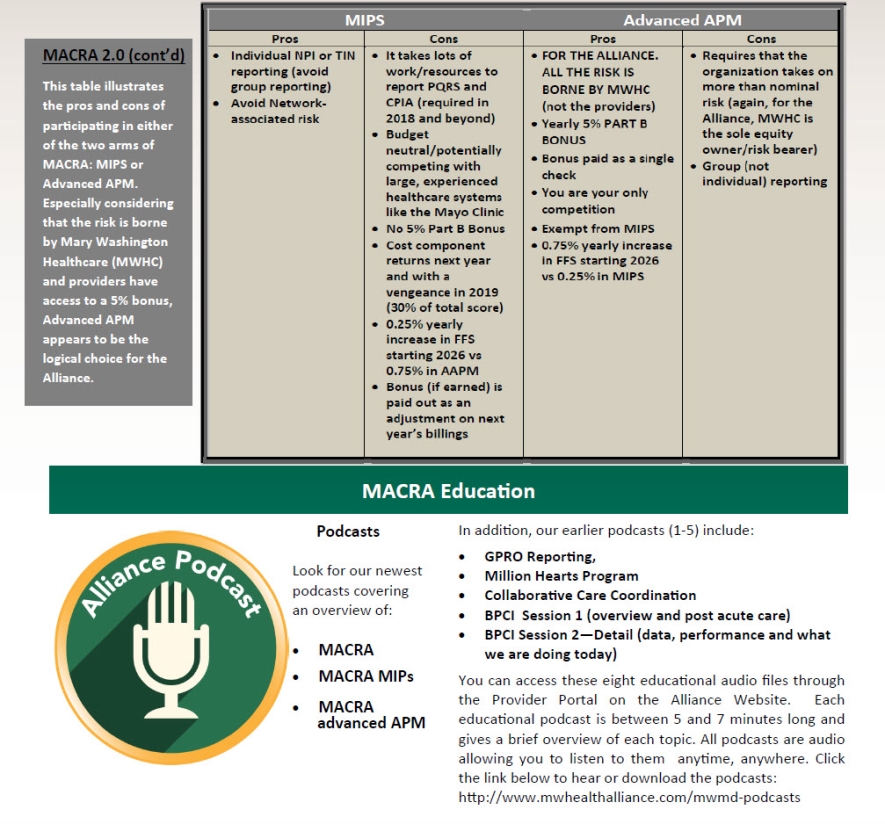
MACRA 2.0
 MACRA went live January 1, 2017. This complex program will guide Medicare
reimbursements for the foreseeable future. There are two major components
of MACRA: MIPS and AAPM. Based upon the features of these programs and
the structure of the Alliance, we feel that AAPM is clearly a better place
for the Alliance than MIPS. But despite multiple educational efforts on
our part last year (Town Halls, newsletters, emails, webinars), our recent
Alliance provider survey revealed that (at least among 72 survey respondents),
MIPS was favored 58% to 42%. Our Communication and Education Committee
has recommended a re-education program that we have dubbed “MACRA
2.0”.
MACRA went live January 1, 2017. This complex program will guide Medicare
reimbursements for the foreseeable future. There are two major components
of MACRA: MIPS and AAPM. Based upon the features of these programs and
the structure of the Alliance, we feel that AAPM is clearly a better place
for the Alliance than MIPS. But despite multiple educational efforts on
our part last year (Town Halls, newsletters, emails, webinars), our recent
Alliance provider survey revealed that (at least among 72 survey respondents),
MIPS was favored 58% to 42%. Our Communication and Education Committee
has recommended a re-education program that we have dubbed “MACRA
2.0”.
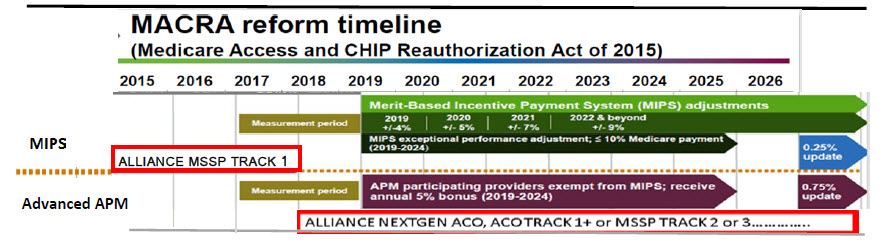
What is MACRA?
MACRA (Medicare Access and CHIP Reauthorization Act) is a federal legislation
signed into law in 2015. It affects healthcare reimbursement because it
repeals the sustainable growth rate (SGR) formula, which determines Medicare
reimbursements; it creates a new framework for rewarding health care providers
for giving better care; and it combines existing quality reporting programs
into one new system.
What is an APM?
An APM (Alternative Payment Model) is a new approach to paying for medical
care that incentivizes quality and value. Examples of APMs included MSSP
(Medicare Shared Savings Program), Bundled Payments and Patient Centered
Medical Homes.
What is an Advanced APM (AAPM)?
Advanced APMs are a subset of APMs that let practices earn more for taking
on sufficient risk related to patients’ outcomes. Examples of AAPMs
in which the Alliance is considering participation include the Next Generation
ACO Model (“NextGen ACO”), MSSP Tracks 2 and 3 and ACO Track 1+.
What is the financial impact of being under an Advanced APM Track?
Physicians in Advanced APMs will receive an annual 5% bonus based on their
Medicare Part B payments. This is in addition to the bonuses or penalties
that are part of the specific Advanced APM in which one is participating.
The provider will also be exempted from MIPS reporting and associated
payment adjustments.
What is “Pick your Pace”?
CMS has provided several options to participate in MIPS in 2017 and avoid
a negative payment adjustment in 2019: (1) “Test the Program”
– report a single quality or improvement activity measure or four
meaningful use-type measures (ACI) and avoid a penalty and earn no bonus
(2) “Report for 90 Days” and avoid a penalty and perhaps earn
a “slight” bonus (3) “Report on Quality, Improvement
Activities and ACI for Full Year” and avoid a penalty and perhaps
earn a “modest” bonus.
What is Merit Based Incentive Program (MIPS)?
The Merit Based Incentive Program is one of two new payment tracks established
by MACRA. It combines parts of the Physician Quality Reporting System
(PQRS), the Value Modifier (VM or Value-based Payment Modifier), and the
Medicare Electronic Health Record Incentive Program into a single program.
Eligible Clinicians will be scored on quality, cost, improvement activities,
and meaningful use of certified EHR technology and a threshold set by
CMS will determine whether clinicians receive a positive (bonus) or negative
(penalty) payment adjustment.